Our New Research on Linking Environmental Data to Health Records
What if your medical record could tell your doctor more than just your blood pressure or past prescriptions? What if it also showed today’s air quality, the week’s temperature forecast, or the safety of your local water supply?
That’s the idea behind our team’s new research, published in the Journal of Medical Internet Research. We explored how environmental data—like heat, pollution, or water quality—could be integrated into electronic health records (EHRs) to make care more responsive to the world around us.
Why the Environment Belongs in Health Records
The environment shapes our health in obvious and subtle ways. Asthma attacks spike on smoky days. Heart problems worsen during heat waves. Water contamination can trigger outbreaks that stretch health systems thin. Yet, most of the time, doctors and nurses don’t have this context in front of them when treating patients.
EHRs have transformed how health information is stored and shared. But so far, they’ve left out a huge piece of the puzzle: the environment patients live in every day.
What We Found
Plenty of data, little connection: Weather stations, satellites, and air quality monitors already generate detailed environmental data. But it rarely makes its way into clinical systems.
Healthcare is still looking backward: Most studies linking environment and health have been done after the fact—useful for research, but not for helping someone in the exam room today.
Barriers are real but solvable: Different EHR systems don’t always talk to each other, privacy protections need to be clear, and there aren’t yet financial incentives for health systems to prioritize this kind of integration.
Potential benefits: If these streams were linked, clinicians could receive alerts when an asthma patient is exposed to wildfire smoke, or public health teams could identify which neighborhoods need extra support during a heat wave.
A Day in the Life Example
Picture a small town in the middle of summer. A heat wave rolls in, and wildfire smoke drifts across the region. Right now, doctors may not know which patients are most at risk until they show up in crisis. But if environmental data were linked into health records, the story could look different:
Clinics could flag patients with asthma or COPD (chronic obstructive pulmonary disease) and send out timely advice.
Community health workers could check in on older adults living without air conditioning.
Local health authorities could direct people to cooling centers before the emergency rooms fill up.
We can use the information we already have to act sooner and prevent illness.
Where We’re Headed
Our team is putting these ideas into practice through the Health and Environmental Record System (HERS). We’re working with clinics to pilot tools that connect environmental indicators—like temperature, air quality, and water quality—to patient records in real time.
In these pilots, providers might get an alert when a patient with asthma is exposed to high pollution, or community teams might identify vulnerable groups during a heat wave. It’s a way of making healthcare climate-smart, practical, and more protective of the patients and communities it serves.
Connecting the Dots:
Health & Environmental Data
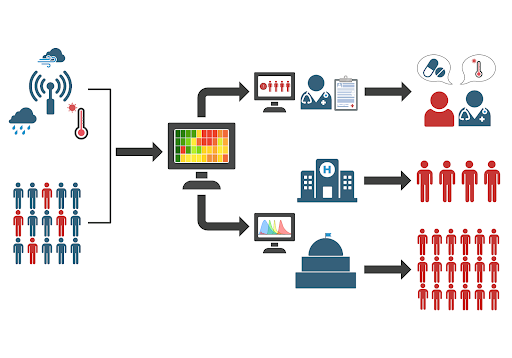
This diagram shows how an integrated electronic health record (EHR) system can combine environmental information from local and remote sensors—such as climate, temperature, and air quality data—with patient health records. The system flags at-risk patients (shown in red) and produces three main outcomes:
For individuals: Clinicians receive actionable insights to provide targeted care, including advice and medication to prevent worsening illnesses.
For the health system: Hospitals can plan resources more efficiently and prepare for spikes in demand.
For government and public health: Officials can make informed policy decisions to protect vulnerable populations and improve public health on a larger scale.
Why This Matters
Environmental risks are no longer rare events—they’re part of daily life for millions of people. By bridging health and environmental data, we have the chance to move from reacting to emergencies to preventing them. And that’s a future worth building.